Bangalore Advanced Urology
WOMEN HEALTH
Safe. Affordable. Ethical Treatments
Urine Leak ( Urinary Incontinence )
Urinary incontinence — the loss of bladder control — is a common and often embarrassing problem. The severity ranges from occasionally leaking urine when you cough or sneeze to having an urge to urinate that’s so sudden and strong you don’t get to a toilet in time.
If urinary incontinence affects your daily activities, don’t hesitate to see your doctor. For most people, simple lifestyle changes or medical treatment can ease discomfort or stop urinary incontinence.
Treatment for urinary incontinence depends on the type of incontinence, its severity and the underlying cause. A combination of treatments may

Behavioural techniques
- Bladder training
- Double voiding
- Scheduled toilet trips.
- Fluid and diet management
Pelvic floor muscle exercises
Your doctor may recommend that you do these exercises frequently to strengthen the muscles that help control urination. Also known as Kegel exercises, these techniques are especially effective for stress incontinence but may also help urge incontinence.
Medications
Medical devices designed to treat women with incontinence include:
- Urethral insert,
- Pessary
Interventional therapies
- Bulking material injections.
- Botulinum toxin type A (Botox).
- Nerve stimulators.
Surgery
If other treatments aren’t working, several surgical procedures can treat the problems that cause urinary incontinence:
- Sling procedures. Strips of your body’s tissue, synthetic material or mesh are used to create a pelvic sling around your urethra and the area of thickened muscle where the bladder connects to the urethra (bladder neck). The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is used to treat stress incontinence.
- Bladder neck suspension. This procedure is designed to provide support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision, so it’s done during general or spinal anaesthesia.
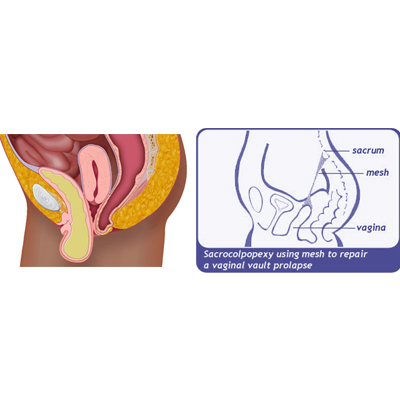
- Prolapse surgery. In women with mixed incontinence and pelvic organ prolapse, surgery may include a combination of a sling procedure and prolapse surgery.
- Artificial urinary sphincter. In men, a small, fluid-filled ring is implanted around the bladder neck to keep the urinary sphincter shut until you’re ready to urinate. To urinate, you press a valve implanted under your skin that causes the ring to deflate and allows urine from your bladder to flow. Artificial urinary sphincters are particularly helpful for men whose incontinence is associated with the treatment of prostate cancer or an enlarged prostate gland.
Recurrent Infection (UTI)
Several factors make women more likely to get recurrent bladder infections, a type of urinary tract infection (UTI). These factors include:
- Kidney or bladder stones
- Bacteria entering the urethra during intercourse
- Changes in estrogen levels during menopause
- An abnormal urinary tract shape or function
- An inherited risk of developing bladder infections (genetic predisposition)
If you’ve had two or more culture-documented bladder infections during a six-month period, consider seeing a urologist — a doctor who specializes in diagnosing and treating urinary tract diseases.

To figure out what’s causing the repeat infections, we recommend:
- Urine culture test of a sample obtained with a catheter
- Visual exam of the bladder and urethra with a lighted scope (cystoscopy)
- Computerized tomography (CT) scan of the urinary tract
Treatment is directed at the underlying cause, when possible. If your doctor can’t find a cause, one of these options may help:
- A long-term, low-dose antibiotic for as long as six months to two years
Intermittent or self-directed antibiotic therapy — for instance, taking an antibiotic after intercourse or starting a course of antibiotics supplied in advance by your doctor at the first sign of a UTI - Vaginal estrogen therapy — if you don’t already take oral estrogen — for signs or symptoms related to vaginal dryness (atrophic vaginitis) after menopause
Expert opinions vary on whether certain lifestyle changes reduce the risk of bladder infection, but it may be helpful to:
- Drink plenty of liquids, especially water, to help flush out bacteria
Urinate often, especially when you feel the need - Wipe from front to back after urination or a bowel movement
- Take showers rather than baths
- Gently wash the skin around your vagina and anus daily using a mild soap and plenty of water
- Use forms of birth control other than a diaphragm and spermicides
- Empty your bladder as soon as possible after intercourse
- Avoid deodorant sprays or scented feminine products in the genital area
Genital Prolapse
Anterior prolapse, also known as a cystocele, occurs when the supportive tissue between a woman’s bladder and vaginal wall weakens and stretches, allowing the bladder to bulge into the vagina. Anterior prolapse is also called a prolapsed bladder.
Straining the muscles that support your pelvic organs may lead to anterior prolapse. Such straining occurs during vaginal childbirth or with chronic constipation, violent coughing or heavy lifting. Anterior prolapse also tends to cause problems after menopause, when estrogen levels decrease.
For a mild or moderate anterior prolapse, nonsurgical treatment is often effective. In more severe cases, surgery may be necessary to keep the vagina and other pelvic organs in their proper positions.
the surgery is performed vaginally and involves lifting the prolapsed bladder back into place, removing extra tissue, and tightening the muscles and ligaments of the pelvic floor. We may use a special type of tissue graft to reinforce vaginal tissues and increase support if your vaginal tissues seem very thin.

Vaginal Fistula Repair
A vaginal fistula is an abnormal opening that connects your vagina to another organ, such as your bladder, colon or rectum. Your doctor might describe the condition as a hole in your vagina that allows stool or urine to pass through your vagina.
Vaginal fistulas can develop as a result of an injury, a surgery, an infection or radiation treatment. Whatever the cause of your fistula, you may need to have it closed by a surgeon to restore normal function.
There are several types of vaginal fistulas:
- Vesicovaginal fistula. Also called a bladder fistula, this opening occurs between your vagina and urinary bladder and is the type that doctors see most often.
- Ureterovaginal fistula. This type of fistula happens when the abnormal opening develops between your vagina and the ducts that carry urine from your kidneys to your bladder (ureters).
- Urethrovaginal fistula. In this type of fistula, also called a urethral fistula, the opening occurs between your vagina and the tube that carries urine out of your body (urethra).
- Rectovaginal fistula. In this type of fistula, also known as a rectal fistula, the opening is between your vagina and the lower portion of your large intestine (rectum).
- Colovaginal fistula. With a colovaginal fistula, the opening occurs between the vagina and colon.
- Enterovaginal fistula. In this type of fistula, the opening is between the small intestine and the vagina.
Most vaginal fistulas require surgery to repair the abnormal opening. we can treat vaginal fistulas with surgery through the vagina or abdomen. Some cases can be treated with minimally invasive surgery (laparoscopic surgery). The location of your fistula determines whether we can perform the procedure through your vagina or your abdomen.
Send us Your Concerns
When you write to us
Kindly provide the following information
- Your name
- Contact number
- Your location
- The specific message to assist you better.
- Are you on hormonal therapy ?
- Have you undergone any surgery for the same problem ?
